What is a urinary tract infection?
A urinary tract infection (also called a “UTI”) happens when bacteria get into the urinary system and multiply. This infection can happen in any part of your urinary system — your kidneys, ureters, bladder and urethra.
Urinary tract is further divided into two sections:
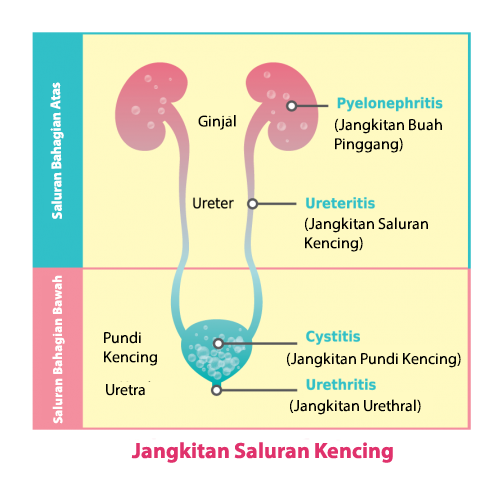
The upper urinary tract is composed of the kidneys and ureters. Infection in the upper urinary tract generally affects the kidneys (pyelonephritis).
The lower urinary tract consists of the bladder and the urethra. Infection in the lower urinary tract can affect the urethra (urethritis) or the bladder (cystitis).
Who are more prone to UTIs?
- Women get UTIs much more often than men. This is because women have a shorter urethra, which may make it easier for bacteria to reach the bladder.
- People with diabetes may have changes in their body’s defense system, making it easier to get urinary infections.
- People with blockages in their urinary tract, such as a kidney stone, are more likely to get UTIs.
- An enlarged prostate gland in a man can also block the flow of urine and cause a UTI.
- People who have a catheter (tube) placed in their bladder for a long time are more prone to UTIs. This is because bacteria on the catheter can infect the bladder.
- Couple who are sexually active. Sexual intercourse can introduce larger numbers of bacteria into the bladder.
What are the symptoms of a UTI?
Most people will have one or more of the following:
- A burning feeling during urination
- An urgent need to urinate, often with only a few drops of urine to pass
- An aching feeling, pressure, or pain in the lower abdomen (stomach)
- Strong odour of the urine
- Cloudy or blood-tinged urine
If the infection spreads to the kidneys and becomes more serious, you may also have:
- pain in the lower back
- fever and chills
- nausea and vomiting
Can anything be done to help prevent UTIs?
The following steps may help:
- Drink plenty of fluids, 8 glasses of water a day.
- Do not postpone going to the bathroom. Urinate when you feel the urge.
- Wipe from front to back to prevent bacteria from the bowels (intestines) from getting into the urinary tract.
- Wash the genital area before and after having sex.
- Regular change of catheter to prevent the growth of bacteria
DON’T
- do not use scented soap/ vagina wash to prevent irritation
- do not hold your pee in if you feel the urge to go
- do not wear tight, synthetic underwear, such as nylon
- do not drink lots of alcoholic drinks, as they may irritate your bladder
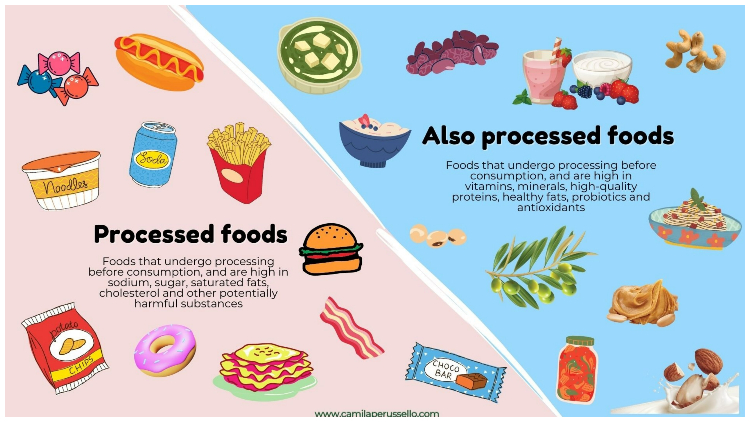
- do not have lots of sugary food or drinks, as they may encourage bacteria to grow
NATURAL HOME REMEDIES FOR UTIS YOU CAN TRY RIGHT FROM HOME
- Cranberry juice
The anthocyanidins and proanthocyanidins (PAC) are tannins found in cranberries and function as a natural defense system against microbes
- Probiotic
probiotics may prevent harmful bacteria from attaching to the urinary tract cells, and may also lower the urine Ph, making it less hospitable to harmful bacteria.
Probiotics are found in supplement form (often a capsule), or they occur naturally in some types of food, including certain yogurts, kombucha, or kefir.
- Eating Garlic
Allicin and other sulphur compounds are thought to be the major antimicrobial factors in garlic.
- Adding vitamin C to your diet
Adequate amount of Vitamin C may also acidify your urine, which limits the growth of some bacteria and may prevent urinary tract infections from occurring.
- Celery juice
Celery extract has antibacterial properties to inhibit the bacterial growth in urinary bladder
Source:
National Kidney Foundation_https://www.kidney.org/atoz/content/uti
https://www.nhs.uk/conditions/urinary-tract-infections-utis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370320/ _doi: 10.6061/clinics/2012(06)18
Universiti Putra Malaysia (UPM). “Using garlic to combat antimicrobial resistant urinary tract infections.” ScienceDaily. ScienceDaily, 10 July 2015.
https://www.medicinenet.com/urinary_tract_infection/article.htm

-520x400.jpg)
.jpg)