Slipped Disc

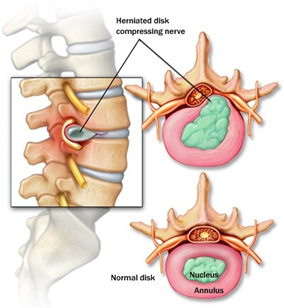
A slipped disc happens when one of the rubbery cushions (discs) that sit between the bones (vertebrae) that stack up spine pushes out from its position. The disc protects the bones by absorbing the shocks from daily activities like walking, lifting, and twisting.
Each disc has two parts: a soft, gelatinous inner portion and a tough outer ring. A slipped disc happens when the inner “jelly” substance pushes through the crack. This is also known as a herniated or prolapsed disc.
Causes
Several factors can contribute to a disc rupture, including:
- Aging – Disc becomes less flexible as people age and becomes more prone to tearing or rupturing
- Gender – Men between the ages of 20 and 50 are most likely to have a slipped disc
- Obesity – Excess body weight causes extra stress on the discs in the lower back
- Occupation – People with physically demanding jobs have a greater risk of back problems
- Sedentary lifestyle – Driving or working at a desk job for long time can increase the risk of a slipped disc
- Smoking – Less oxygen is supplied to the disc and it may lead to rapid degeneration of the discs

Symptoms
Slipped discs can happen anywhere along the spine, but slipped discs most often occur in the lower back or the neck. It’s rare for a slipped disc to be in the mid-back. However, not all slipped discs cause symptoms. Many people will never know that they have slipped a disc.
Slipped disc at the lower back
It’s common for a slipped disc at the lower back to cause “sciatic nerve” pain. This sharp pain usually radiates from the buttock to the leg and sometimes to the foot. Other symptoms of a slipped disc at the lower back include:
- Back pain
- Tingling or numbness in the legs and/or feet
- Muscle weakness
Slipped disc at the neck
Symptoms of a slipped disc at the neck include:
- Pain near or between shoulder blades
- Pain that travels to shoulder, arm and sometimes hand and fingers
- Neck pain, especially in the back and on the sides of the neck
- Pain that increases when bending or turning the neck
- Numbness or tingling in the arms
Treatment
In most cases, slipped discs do not require surgery. With time, the symptoms of a slipped disc will improve in approximately 9 out of 10 people. However, time taken to improve varies, ranging from a few days to a few weeks.
Nonsurgical treatment
Initial treatment for a herniated disc is usually nonsurgical. Nonsurgical treatment may include:
- Applying heat or cold. Initially, cold packs can be used to relieve pain and inflammation. After a few days, might switch to gentle heat to give relief and comfort.
- Rest. Take rest breaks throughout the day but avoid sitting for long periods. Try to avoid activities that worsen the pain.
- Resuming activity slowly. Make sure movements are slow and controlled, especially bending forward and lifting.
Medication
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as ibuprofen or naproxen can help relieve pain by treating inflammation in the nerves and soft tissues surrounding the disc.
- Neuropathic drugs. These drugs affect nerve impulses to decrease the pain. They include gabapentin (Neurontin), pregabalin (Lyrica), duloxetine (Cymbalta), or venlafaxine (Effexor XR).
- Muscle relaxants. These medications can calm spasms and ease pain. Sedation and dizziness are common side effects.
- Steroid injection. An injection of a cortisone-like medicine into the space around the nerve may provide short-term pain relief by reducing inflammation.
Physical therapy
Strengthening the core—the muscles in the back, abdomen, upper thighs, and buttocks—is an important part of therapy to treat symptoms of a slipped disc. If these muscles are weak, the spine bears more weight. This added pressure could cause instability or worsen an existing spine problem. A physical therapist can recommend a series of exercises for strengthening these core muscle groups, which can improve posture, relieve pressure on the nerves affected by a slipped disc, and alleviate pain.
Surgical treatment
A doctor may recommend surgery if conservative treatment options, such as physical therapy and medications, do not reduce or end the pain altogether. The benefits of surgery should be weighed carefully against its risks. Although a large percentage of patients with herniated discs report significant pain relief after surgery, there is no guarantee that surgery will help.
A patient may be considered a candidate for spinal surgery if:
- Pain limits normal activity or impairs quality of life
- Progressive neurological deficits develop, such as leg weakness and/or numbness
- Loss of normal bowel and bladder functions
- Difficulty standing or walking
- Medication and physical therapy are ineffective
- The patient is in reasonably good health
Complications
Left untreated, a slipped disc may lead to complications such as:
- Worsening symptoms, such as increased pain, numbness or weakness that can affect daily routine
- Loss of bladder control or bowel control, which may lead to incontinence or difficulty urinating
- Saddle anesthesia, where the slipped disc compresses the nerves and leads to loss of sensation in the inner thighs, back of the legs and around the rectum
- Permanent nerve damage, which may lead to permanent weakness or paralysis
Prevention
- Using proper lifting techniques
Position your feet shoulder-width apart
Bend your knees and keep your back straight
Use your legs to lift you up
Keep the object close to the center of your body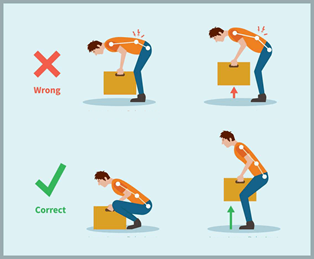
- Practicing good posture
When standing, keep your shoulders aligned over your hips
Avoid slouching, especially while sitting at your computer
Sit with your feet flat on the floor and your knees bent at 90-degree angles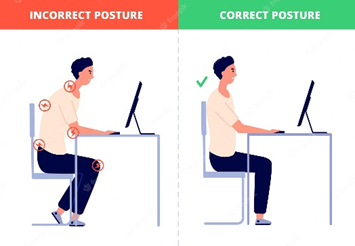
- Exercising regularly
- Focus on workouts that strengthen back and abdomen muscles to support your spine
Avoid exercises such as squats, sit-ups, and high impact aerobics activities
- Maintain a healthy weight
Being overweight or obese puts excessive pressure and strain on the back and knees. It also may contribute to poor posture
- Quit smoking
Smoking deprives healthy tissue of nutrients and oxygen, increasing the risk of developing spinal disc degeneration and osteoporosis. A smoker’s heavy coughing bouts can also increase pressure on the spine
References
1. Cleveland Clinic (2021). Herniated Disk (Slipped, Ruptured or Bulging Disk). Retrieved 10 June 2023, from https://my.clevelandclinic.org/health/diseases/12768-herniated-disk .
2. Mayo Clinic (2022). Herniated disk. Retrieved 10 June 2023, from https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095 .
3. Nall, R. (2017). Slipped (Herniated) Disc. Retrieved 10 June 2023, from https://www.healthline.com/health/herniated-disk .
4. Park, D. K. (2022). Herniated Disk in the Lower Back. Retrieved 10 June 2023, from https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disk-in-the-lower-back/ .
5. Portal Rasmi MyHEALTH (2019). Slipped Disc of Spine. Retrieved 10 June 2023, from http://www.myhealth.gov.my/en/slipped-disc-spine/ .