Dialysis is a type of treatment that helps our body to remove extra fluid and waste products from the blood when the kidneys are failed to function normally. Dialysis can be done in hospitals, dialysis centres, or at home. For severe cases of Acute Kidney Injury (AKI), dialysis treatment is required for a short time until kidney function is recovered. However, for kidney failure or end-stage kidney disease (ESKD), dialysis is crucial for the rest of life or until the patient can opt for a kidney transplant.
Dialysis performs the duties that the kidney usually does to keep the body in balance, such as:
- Removing waste and extra fluids in the body to prevent them from building up in the body
- Keeping safe levels of minerals in the blood, such as potassium, sodium, calcium, and bicarbonate
- Helping to regulate blood pressure
People who receive dialysis treatment need to be mindful of what they eat. The specific meal plan recommended for them may vary depending on their routine and lifestyle.
Between dialysis sessions, wastes can build up in the blood and make the patient unwell. Patients can reduce waste build-up by controlling some nutrients in their daily intake. Some foods cause waste to build up quickly between dialysis sessions. If the blood contains too much waste, the kidney treatment session may not remove them all.
For dialysis patients, the healthcare practitioners will recommend controlling the following nutrients:
1. SODIUM

Sodium is a major constituent of many food items especially, in table salt. For dialysis patients, the kidneys are unable to drain out the excess sodium. Therefore, it is recommended to take sodium less than 2,000 gm per day.
Tips to reduce sodium:
- Limit choice of foods like keropok, salty biscuits, nuts, potato chips, french fries, salted fish/egg/vegetable and pickles.
- Do not add salt or monosodium glutamate (MSG) if possible when cooking. Seasoned foods with natural herbs and spices such as pepper, chili, lemon grass leaves, pandan leaves, coriander, or curry leaves.
- Avoid belacan, budu, tempoyak and cencaluk.
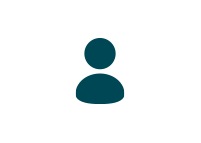
- Avoid processed food that high in sodium like cheese, bacon, sausage, ham, hot dogs or pepperoni. Limit processed beef, pork or poultry.
- Omit salad dressing, condiments, sauces and gravies. Consider use lime/lemon juice or vinegar as salad dressing.
- Choose fresh meat fish or poultry prepared without sauces or gravies. Limit salty sauces such as soy, teriyaki, barbecue, oyster, chili, tomato, and steak.
- Limit or avoid broth, cream soup or soups prepared with stock cubes.

2. POTASSIUM
Although potassium is crucial for the body, dialysis patients should limit it. Recommended intake is less than 2,000 gm of potassium per day. Consuming the right amount of potassium in your blood can maintain your heart beating at a steady pace. Potassium levels can rise between hemodialysis sessions and affect your heartbeat. Too much potassium can be dangerous to your heart and even fatal.
Tips to control potassium intake:
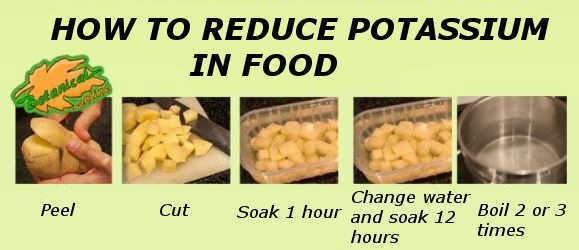
- Potassium is soluble in water. Cutting vegetables into small pieces and soaking them for 1-2 hours in several changes of warm water will help leach out of potassium content.
- Drain away liquid from canned fruits and vegetables.
- Peel off the skin from fruits.
- Use whole rather than ground spices for flavoring.
- Avoid herbal and traditional remedies such as ginseng roots, banana stem, akar kayu and others.
3. PHOSPHATE
The recommended intake for phosphate is less than 800 mg to 1000 mg per day. Too much phosphate in the blood pulls calcium from bones. Losing calcium may result in weak and brittle bones subsequently will increase the risk of fracture. Also, too much phosphate may cause itchiness to the skin. Kidney patients are advised to take a phosphate binder to control the phosphate level in blood between hemodialysis sessions.
Tips to control phosphate intake:
- Avoids eating the cartilage and soft bones of fish, shellfish and meat.
- Reduce intake of cocoa, chocolate-based beverages and cola drinks.
- Limit dairy food products such as milk, curd/yogurt and cheese. Use non-dairy creamer to replace milk in beverages.
- Phosphate binders must be taken with meals. For calcium carbonate, it is best to chew the tablets.
- If forgotten, phosphate binders can be eaten within 15 minutes after meal. Otherwise, it should be left out and the dose will not be doubled at the next meal.
Dialysis patients need to bring their phosphate binders when eating out at all times.
4. PROTEIN

For non-dialysis patients, they are advised to follow a low-protein diet. Being on dialysis, they are encouraged to eat high protein diet. Protein helps to restore muscle strength and repair tissues. Besides, a high-protein diet is crucial to fight infections and speed up healing from surgery. Eating high-quality protein is encouraged because it produces less waste for removal during dialysis. High-quality proteins come from meat, poultry, fish, and eggs. Avoid processed meats such as hot dogs and canned chili, which have high amounts of sodium and phosphorus.
5. LIQUID
Dialysis patients need to keep track of their liquid intake. Excess fluid can build up in the body, therefore causing swelling and weight gain between dialysis sessions. Besides, fluid buildup can affect blood pressure and subsequently burden the heart to work harder, which might lead to fatal heart conditions. Other than the heart, our respiratory function also can be threatened if fluid is excessive.
Tips to control thirst:
- Identify the cause of frequent thirst
- Gurgle often
- Consume frozen cubed fruits
- Use a mist sprayer to moisturize the mouth
- Chew on sugar-free chewing gum
- Cease smoking
- Avoid too salty or sweet food
6. SUPPLEMENTATION

Dialysis patients may not get enough vitamins and minerals in their diet because they have many nutrient restrictions from food. Healthcare providers may prescribe them with suitable vitamins and mineral supplements. For safety reasons, it is highly encouraged to take supplementation only when needed and under close supervision of healthcare providers.
Supplementation that is safe for dialysis patients:
- B-complex: to aid red blood cell formation
- Iron tablet: to increase haemoglobin level
- Vitamin C (low dose: below 250mg): to enhance absorption of iron
- Vitamin D:to maximize absorption of calcium to bone
- Calcium: to strengthen bone, consume together with phosphate binder to prevent calcium-phosphate clump in blood.
Avoid supplement that contain:
- Vitamin A, E & K: These vitamins can cause build-up in the blood and harm the body.
- Herb-based remedies: May create interaction with prescribed medication and causes side effects.
- Megadose of vitamin C: Large doses of vitamin C produce by-product called oxalate that will deposit in bones and soft tissues subsequently result in painfulness.
REFERENCES
Malaysian Dietitians’ Association. Medical Nutrition Therapy Guidelines for Chronic Kidney Disease, 2005.
Ministry of Health. Clinical Practice Guidelines: Management of Chronic Kidney Disease in Adults, 2011
National Kidney Foundation (n.d). Dialysis. Retrieve May 7, 2023 from https://www.kidney.org/atoz/content/dialysisinfo
National Kidney Foundation (n.d). Dietary Guidelines for Adults Starting in Hemodialysis. Retrieve May 7, 2023 from https://www.kidney.org/atoz/content/dietary_hemodialysis
National Institute of Diabetes and Digestive and Kidney Diseases (2016). Eating & Nutrition for Hemodialysis. Retrieve May 7, 2023 from https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition
Paresh K.J. (2019). Diet and Nutrition for Kidney Patients. Retrieve May 7, 2023 from https://healthlibrary.askapollo.com/diet-and-nutrition-for-dialysis-patients/
Zhang KY, Zuo L. (2014). Vitamin C supplementation in patients on maintenance dialysis. World J Clin Urol. 3(3): 344-350. DOI: 10.5410/wjcu.v3.i3.344