Diabetic Foot Ulcer
INTRODUCTION
Diabetic foot is one of the most devastating complications of diabetes, which is defined as infection, ulceration or destruction of tissues at the foot. It is usually the result of poor glycemic control, underlying nerve damage, peripheral vascular disease, or poor foot care.
According to World Health Organization, the global prevalence of diabetes among adults of > 18 years old has risen from 4.8% in 1980 to 8.5% in the year of 2014. As the numbers of newly diagnosed diabetics increase yearly, the incidences of foot ulcer also increase.
ETIOLOGY
The etiology of diabetic foot ulcer is multifactorial, however the common underlying causes are:
- Poor blood sugar control
- Formation of calluses
- Foot deformities
- Improper foot care
- Underlying nerve damage / poor blood circulation of lower limbs
- Dry skin
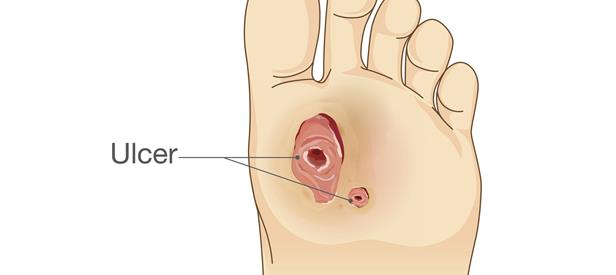
PRESENTATION OF THE WOUND
- Well defined wound
- Punch out-look
- Surrounding skin will often be calloused
- Depth of wound typically depending on the thickness of callous

The most common cause of ulceration is due to repetitive mechanical forces of gait, which lead to callus (pre-ulcerative lesion). When the callus becomes too thick, the callus will press on the soft tissues underneath which eventually lead to ulceration.
A layer of whitish, macerated, moist tissue found under the surface of the callus indicates that the foot is close to ulceration, and urgent removal of the callus is necessary.
Figure 1 showing diabetic ulcer revealed underneath of callus.

TREATMENT
PHARMACOLOGICAL TREATMENT
Oral Analgesic
Simple pain killer ( e.g. paracetamol or NSAIDs) should be considered in mild and moderate pain in diabetic foot ulcer patient.
- Topical antibiotic
Topical antibiotics are used to treat infected wound or to further prevent infection in uninfected wound.
- Oral Antibiotic
Oral antibiotic will be prescribed by physician when there are systemic symptoms of infection in diabetic foot ulcer patient.
NON PHARMACOLOGICAL TREATMENT
Wound care
Wound care is important in management of diabetic foot. There are different types of wound dressing which helps in reduce symptom, provide wound protection and improve wound healing. It has 3 important steps in diabetic wound management:
- Debridement
Debridement is a process of removing debris and surrounding callus that will slow down wound healing and causes infection.
- Offloading
Offloading is the process of redistribution the pressure off the wound to the entire weight-bearing surface of the foot. It can be achieved by either wearing temporary footwear until ulcer heal or wearing pressure-relief devices
Mechanical loading of feet during daily activities, e.g. walking or standing which exposes pressure on plantar surface causing compression and shear stress. This pressure and stress will be aggravated by foot deformities ( e.g. hammer and claw toes) which are very common in diabetic patients. Therefore patients are advised on using footwear that fits, protects and accommodates the shape of feet (with socks). Patient who are at moderate or high-risk are usually prescribed with footwear with removable cast boots to decrease the pressure on affected area. It has to ensure that it fits, protects and supports the foot.
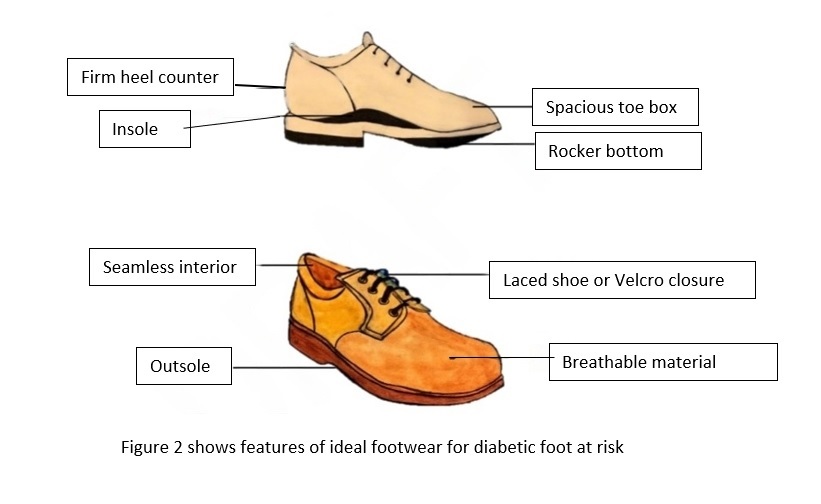

Figure 3 shows example of removable cast boots for patient with diabetic foot ulcer.
c. Appropriate wound dressing
- Dry wound needs topical application that add moisture to the wound
- Diabetic wound with heavy exudates needs a dressing to absorb moisture.
- Dressings need to be changed at least daily in order to apply clean wound covering & monitor infected wound.

Supplementation
Vitamin B12
Vitamin B12, which is also known as cobalamin is vital for proper functioning and development of nervous system. Nerve damage with symptoms of pain, tingling, numbness and loss of sensation is often associated with Vitamin B12 deficiency.
Metformin, which is one of the diabetic agent commonly used for diabetic patient has confirmed that its long term use has contributed to vitamin B12 deficiency in patient with diabetic disease. Metformin has been reported to lead to malabsorption of vitamin B12. Therefore, diabetic patient who is taking metformin is encouraged to consume vitamin B12 through diet or supplement. This is to prevent development of nerve damage which eventually leads to foot ulcer.

PREVENTION
Patients who are at high risk of developing diabetic foot ulcer need to know the basic care of foot, callus and nail, this should be done regularly to prevent foot problems. Diabetic foot prevention can be done by:
- Lifestyle modification
- Having good glycemic and blood pressure control by taking medication, follow diet plan, exercise regularly, and monitor blood sugar regularly through HbA1c test is important to reduce the incidence of diabetic foot ulcer and subsequent risk of amputation.
- Smoke cessation
- Do not smoke as it reduce blood flow in feet.
- Take good care of feet hygiene by washing them daily with mild soap. Use only lukewarm (below 37°C) and not hot water. Do not soak feet as it can cause dry skin.
- Use moisturizer daily to keep dry skin from itching or cracking. But do not moisturize between the toes as it could risk an infection to occur
- Cut toenails carefully after washing and drying the feet. Do not cut nails too short as this could lead to ingrown toenails.
- No self-treat corns or calluses.
- Wear clean and dry socks which are not too tight and are light coloured. Socks with extra cushioning, no elastic top, higher than ankle, made from fibers material are preferred.
- Never walk barefoot indoors or outdoors.
- Put feet up when sitting to ensure good blood circulation. Keep the blood flowing to feet by wiggling toes and moving ankles for five minutes, 2 – 3 times a day. Don’t cross legs for long periods of time.
- Seek for treatment if there is presence of pain, noticeably red or discolored areas, discharge, bad smell, ulcer, blister or if feeling generally unwell with difficulty controlling blood sugar level
REFERENCE
- Ministry of Health Malaysia. Clinical practice guideline: Management of diabetic foot. 2nd ed. Ministry of Health Malaysia. http://www.moh.gov.my/. 2018.
- Edmonds ME, Foster AV. ABC of wound healing: Diabetic foot ulcers. BMJ. 2006 May 1;332(Suppl S5).
- MIMS Malaysia. Infectious Disease: Diabetic Foot Infection. https://specialty.mims.com/diabetic%20foot%20infection/signs%20and%20symptoms?channel=infectious-diseases.
- Badedi M, Darraj H, Hummadi A, Solan Y, Zakri I, Khawaji A, Daghreeri M, Budaydi A. Vitamin b12 deficiency and foot ulcers in type 2 diabetes mellitus: A case–control study. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2019 Dec 6:2589-96.