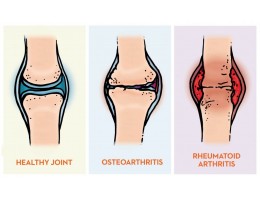
Osteoarthritis (OA) is a type of joint disease that happens when the cartilage between bones that cushions the joints wears down. It is the most common form of arthritis known as degenerative joint disease or “wear and tear” arthritis. It commonly affects hands, knees, hips and spine.

What are the risk factors for OA ?
There are several risk factors for osteoarthritis, and the main risk factors is advancing age. High body mass index or obesity will also increase the risk getting osteoarthritis due to extra weight that put more stress on the joints. Besides, osteoarthritis might also happen because of trauma or overuse such as previous knee injury or repetitive stress on joint. Women are more likely to develop osteoarthritis than men especially those with menopause. Apart from that, genetics also will increase the chance to have OA, for example people who have family members with OA are more likely to develop OA or people who have hand OA are more likely to have knee OA.
Symptoms of Osteoarthritis includes:
- Pain. Affected joints might hurt during or after movement.
- Stiffness. Joint stiffness might become noticeable upon awakening or after being inactive
- Swelling. Soft tissue inflammation around the joint
- Tenderness. Joint will feel tender when pressure apply onto or near it.
- Grating sensation. Might hear popping or crackling when using the joint.
- Bone spurs. Hard lumps can form around the affected joint.
- Loss of flexibility. Not able to move the joint through its full range of motion.
How is osteoarthritis being treated?
Pharmacological treatment
Pharmacological treatment for osteoarthritis can be subdivided into Oral Treatment, Intra-articular Treatment and Topical Treatment. All these treatments should be done under advice and supervision from medical professional.
The treatment will usually begin with oral treatment like acetaminophen (paracetamol) as first line and continue if still effective or step up to NSAID (non-steroidal anti-inflammatory medication). Start NSAID therapy, beginning with ibuprofen or naproxen; switch to different NSAID like diclofenac sodium, meloxicam etc if initial choice is not effective. Acetaminophen (paracetamol) is more prefer for treating mild osteoarthritis while NSAID is given to treat moderate to severe osteoarthritis.
Intra-articular treatment like intra-articular injection of corticosteroid and intra-articular injections of hyaluronic acid (viscosupplementation) are another option for treating osteoarthritis. They have proven effectiveness in osteoarthritis of knee. Corticosteroid injection provides short-term relief lasting 4 to 8 weeks and is used for acute exacerbation while hyaluronic acid injection provides long term relief and is used for persistent knee osteoarthritis.
Topical treatment in the form analgesic patches, creams, rubs or sprays may be applied over the skin of affected area to relieve pain.
Non Pharmacological Treatment
- Weight management
If patient with osteoarthritis is obese, it is important to reduce weight. Reduction of weight will help in pain reduction and improvement of knee function.
- Physiotherapy and occupational Therapy
Physiotherapy and occupational Therapy is also the recommended treatment of osteoarthritis. These therapies are individualised and might be different for everyone. The main purposes for both the therapies are to increase muscle strength, balance, coordination and joint mobility, therefore improve in pain management and resume normal physical activity.
- Exercise
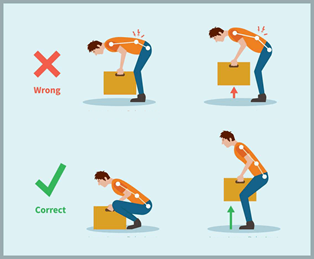
Exercise is important to improve flexibility, joint stability and muscle strength. Activities like swimming, aerobics and low impact strength training are recommended. Avoid excessive and vigorous exercises as they may increase the symptoms of arthritis.
- Joint Support and Appropriate Foot ware
For patient who suffer from osteoarthritis, joint support and appropriate foot ware will aid in supporting the joints, reduce burden on the joints and therefore protect the joints from further damages.
- Hot and cold therapies
Intermittent hot and cold treatments may provide temporary relief of pain and stiffness. Such treatment include a hot shower and application of hot or cool gel.
Rheumatoid Arthritis
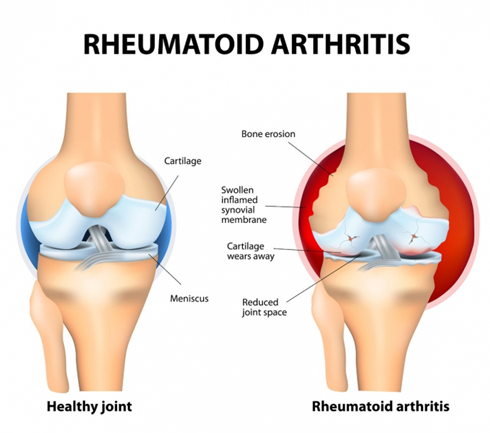
Rheumatoid arthritis (RA) is a chronic, progressive autoimmune disease where immune system attacks healthy cells in body by mistake causing inflammation of the joints. Bone erosion, destruction of cartilage and complete loss of joint integrity might happen if rheumatoid arthritis is left untreated for prolonged period. RA usually affects the hands and feet first but it can occur in any joint and is usually involves the same joints on both sides of the body.
Risk Factors
- Age. RA can begin at any age but the likelihood increase with age.
- Gender. Women tend to have higher possibility to develop RA than men.
- Genetics. People born with specific genes (HLA = Human Leukocyte Antigen) are more likely to develop RA.
- Smoking. Cigarette smoking increase the risk of developing RA and make the disease worse.
- Obesity. Being obese can increase the chance the developing RA
Signs and symptoms
- Pain in more than one joint
- Stiffness in more than one joint that lasts longer than 30 minutes
- Swelling in more than one joint
- Symmetrical joint involvement (such as in both hands or both knees)
- Joint deformity
- Loss of function and mobility
- Unsteadiness when walking
Pharmacological Treatment
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
NSAIDS are commonly used as pharmacological treatment in rheumatoid arthritis to reduce pain and inflammation in RA.
Corticosteroids
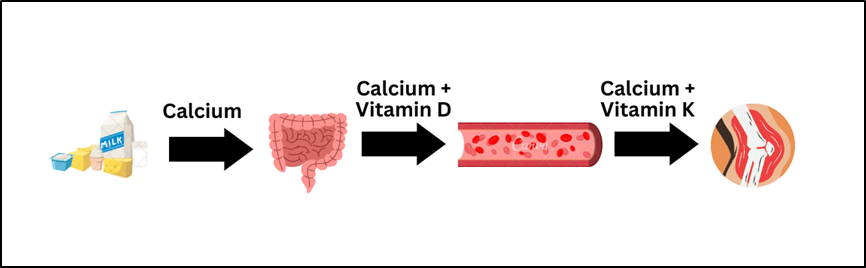
Corticosteroids are used to reduce inflammation in RA. But the long-term use of corticosteroids will result in certain complications such as osteoporosis and infection. Calcium and Vitamin D supplementation will be recommended in such cases.
Disease Modifying Anti-Rheumatic Drugs (DMARDs)
DMARDs will also be given in the treatment of moderate to severe Rheumatoid Arthritis. It affects how the immune system works hence slowing down the progression of rheumatoid arthritis and prevent permanent damage to the joint and other tissues. A person usually takes a DMARD for life. Methotrexate is an example of DMARD.
Non Pharmacological Treatment
Patient Education
In the management of Rheumatoid arthritis, patient education plays important role to allow patients understand further about the disease. This includes information of the diagnosis, nature of the disease including its complications and, benefits and risks of therapeutic options. Giving education to patient will increase the adherence of the patient to the therapy and to achieve the goal of the treatment.
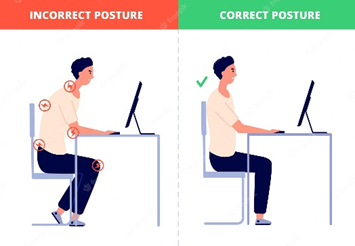
Occupational Therapy and Physiotherapy
The main purpose is to manage the pain and maintain joint functions. Occupational Therapy can help a person learn new and effective ways of carrying out daily tasks to minimise stress to painful joints. Physical therapy will advise people on using the assistive devices like cane and help individual to develop suitable exercise plan.
Stop smoking
Cigarette smoking can make the disease worse and make it more difficult for someone to stay physically active. Hence stop smoking is able to improve the quality of life of patient with rheumatoid arthritis.
Maintain a healthy weight
Being obese can put more stress on the joints. Hence maintaining a healthy weight is important to reduce exacerbation of rheumatoid arthritis.
Supplements for Osteoarthritis (OA) and Rheumatoid arthritis (RA)
- Glucosamine:
Glucosamine is used by the body to build tendons, ligaments, cartilage and joint. Therefore, taking glucosamine supplement will help to improve mobility for patient with osteoarthritis.
- Chondroitin:
Chondroitin provides the joints with elasticity.
- Type II collagen:
Help to maintain healthy cartilage by creating a balance between continuous process of cartilage degradation and renovation.
- Soy Boswellia:
Natural inflammatory phytonutrient. Support normal joint functions and mobility.
- Sodium Hyaluronate :
Possess anti-inflammatory and anti-edematous properties. It strives to improve joint pain by restoring the cushioning of joints and increasing the supplies of synovial fluid that help in lubrication of joint.
- Turmeric
Consist of curcumin that helps to protect cells from damaging by free radicals. It is reported to have beneficial effects on joint health due to its antioxidant properties.
Differences Between Osteoarthritis (OA) and Rheumatoid Arthritis (RA)
| Osteoarthritis | Rheumatoid Arthritis |
| OA is a degenerative, wear and tear type of disorder. | RA is an autoimmune disease. |
| Usually affect people over 40 years old. | Usually affect people around 35-45 years old. |
| Pain is worsened after prolonged use of the joint. | Stiffness and pain become worse after being inactive and usually lasts for 30mins. |
| Involve one particular joint or area. | Involve multiple joints all over the body. |
| Do not required immune suppressant medicine. | Required immune suppressant medicine. |
References:
1. Osteoarthritis (OA) | Arthritis | CDC [Internet]. Cdc.gov. 2020 [cited 3 December 2021]. Available from: https://www.cdc.gov/arthritis/basics/osteoarthritis.htm
2. Sinusas K. Osteoarthritis: Diagnosis and Treatment [Internet]. Aafp.org. [cited 3 December 2021]. Available from: https://www.aafp.org/afp/2012/0101/p49.html
3. Osteoarthritis: Symptoms, Causes and Treatment [Internet]. Cleveland Clinic. [cited 3 December 2021]. Available from: https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
4. [Internet]. Mangament of Osteoarthritis Second Edition. Moh.gov.my. 2013 [cited 1 December 2021]. Available from: https://www.moh.gov.my/moh/attachments/8933.pdf
5. [Internet]. Management of Rheumatoid Arthritis.Www2.moh.gov.my. 2019 [cited 1 December 2021]. Available from: https://www2.moh.gov.my/moh/resources/Penerbitan/CPG/Rheumatology/QR_RA_17052021.pdf
6. Rheumatoid arthritis (RA): Symptoms, treatments, causes, and more [Internet]. Medicalnewstoday.com. 2021 [cited 3 December 2021]. Available from: https://www.medicalnewstoday.com/articles/323361#treatment
7. Rheumatoid Arthritis (RA) | Arthritis | CDC [Internet]. Cdc.gov. 2020 [cited 3 December 2021]. Available from: https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
8. Osteoarthritis and Rheumatoid Arthritis Differences Archives – Pediaa.Com [Internet]. Pediaa.Com. 2016 [cited 5 December 2021]. Available from: https://pediaa.com/tag/osteoarthritis-and-rheumatoid-arthritis-differences/