Health Articles
Find out more about your health here from our health professionals!

Glaucoma

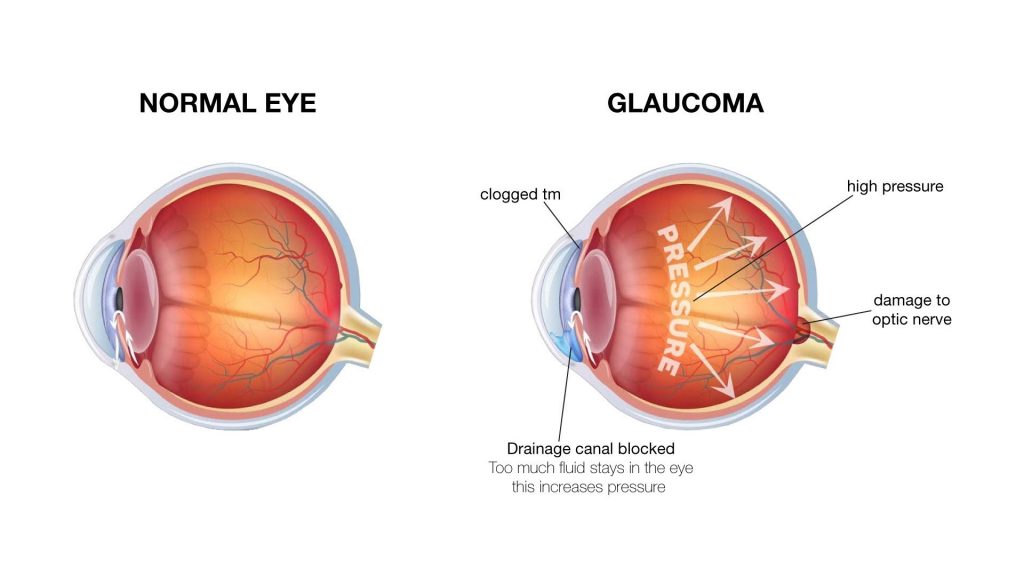
Glaucoma is a disease involving the optic nerves of the eyes- usually affecting both of the eyes. It usually occurs when there is an escalation of pressure in the eyes. Our eyes usually produce a protective fluid (that surrounds the tissues of the eyes) also known as aqueous humour. An optimum eye pressure is achieved when the amount of fluid produced is equivalent to the amount of fluid being drained out of the eyes. If there is any slight blockage in the outflow channel, the pressure in the eyes rises due to the accumulation of the fluid surrounding the eyes.
There are several distinguished types of glaucoma; one being acute or close-angle glaucoma that is rare and occurs due to a sudden, high increment in the eye pressure which causes pain. Another type being chronic or open-angle glaucoma which occurs gradually and is often left undetected due to the absence of any signs or symptoms. Next, secondary glaucoma is caused by an inflammation of the middle layer of the eyes. Another type of glaucoma would be childhood or congenital glaucoma which is extremely rare and only occurs in very young children due to abnormalities in the eyes.
A few risk factors increase the chances of developing glaucoma. One of them is family history which means if your parents or siblings have glaucoma, you have a significant risk of developing it as well. Another risk factor would be age– the older you are, the higher the risk of developing glaucoma. Ethnic groups also play a role in increasing the chance of developing glaucoma, in which people who are of Afro-Caribbean and African descent will have a higher risk of developing glaucoma. Other than that, short sightedness can also make you more prone to develop glaucoma. Diabetes also appears to be another risk factor of developing glaucoma.
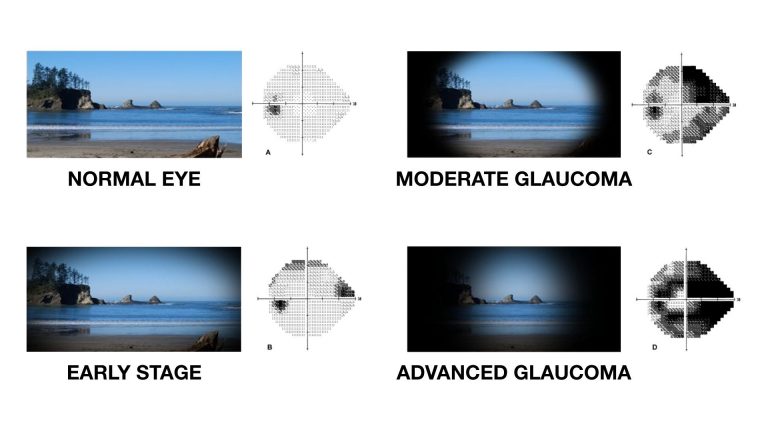
Oftentimes, glaucoma goes undetected due to absence of signs and symptoms in the early stages. Given the situation that you have acute or open-angle glaucoma, it will take a long time before your eyesight deteriorates. When a person experiences blurred vision, dull pain around the head, nausea or vomiting or seeing a glare or shadow around the light of a lamp, he or she is usually at a severe level and require guidance from an ophthalmologist with urgency. Therefore for those that have a higher risk for developing glaucoma, it would be advisable to undergo an eye examination yearly. After all, prevention is better than cure.
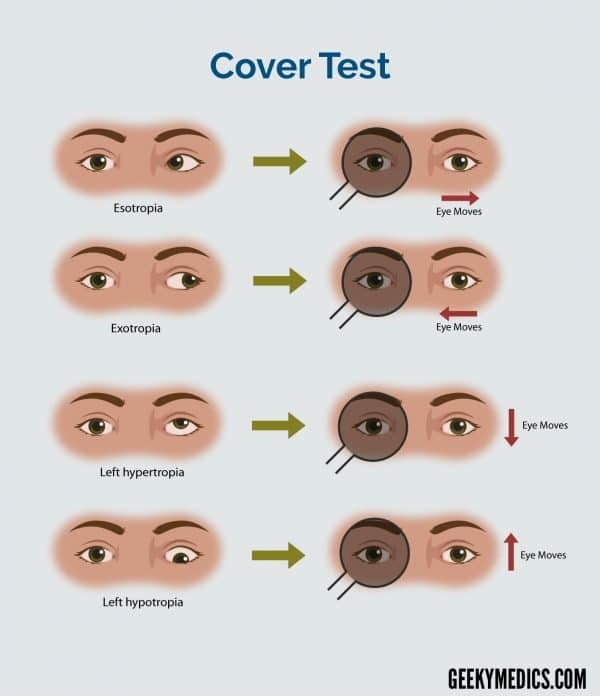
Thus, eye tests that are simple and painless should be performed regularly for early detection. Firstly, an eye pressure test in which a local anesthetic eye drop will be placed in both of the eyes before a small instrument is gently placed against your eye to measure the intraocular pressure of the eyes.
 Eye pressure test
Eye pressure test
Next, optic nerve examination can be conducted to examine the condition of your optic nerves.
A visual field test can also be performed to test for the missing areas of peripheral vision in which patients will click a button when they see a light flash upon displays of various light spots.
Once damage is done to the vision by glaucoma, it is hardly reversible. However, there are treatments that can prevent the eye-sight from going worse. The go-to treatment for acute or open-angle glaucoma is eye drops that patients need to use for lifelong. In the early stages of glaucoma, these eye drops can help control the eye pressure and therefore prevent further damage to the eyes. The effectiveness of the eye drop will be determined by the ophthalmologist upon regular glaucoma checks. If the use of eye drops is unable to control glaucoma, laser procedures can help to drain the fluid out of the eye effectively or surgery on the draining channel can be performed as well.
Certain lifestyle habits can be easily adapted to reduce the severity of glaucoma. Firstly, limit caffeine intake as caffeine can increase the pressure of the eyes. Next, limit alcohol intake as excessive drinking of alcohol can damage optic nerves. Fish oil supplements can help to improve eye health as well. Exercising cautiously can help to improve glaucoma and general health. Other than that, sleeping with your head on a pillow can help to reduce eye pressure as well.
References
- Ow Yong, S.E. (2021). [Comparison of normal eye with glaucoma eye]. Vista Eye Specialist. https://www.vista.com.my/pages/2021/02/17/glaucoma/
- Salmon, J. (2015) Glaucoma information for patients. Available at: https://www.ouh.nhs.uk/patient-guide/leaflets/files/11826Pglaucoma.pdf
- NHS. (2021). Glaucoma. Available at: https://www.nhs.uk/conditions/glaucoma/
- Glaucoma UK. (2021). Living with Glaucoma. Available at: https://glaucoma.uk/care-support/living-with-glaucoma/
- Othman, S. (2019). Glaukoma. Available at: http://www.myhealth.gov.my/dewasa-glaukoma/
-260x200.jpg)
Digital eye strains (DES)
.jpg)
As the science and technology become more and more developed nowadays, people are unable to live without digital devices like smartphones, laptops etc. Even students are also using smartphone, tablets or laptops for online classes, especially during COVID-19 pandemic, which has increased the exposure to digital devices. The usage of these digital devices has become a huge part of modern life.
But, do you know that, looking at these digital devices for many hours per day can actually cause a significant stress to your eyes and eventually develop into an eye disease. This is known as digital eye strains. This has increased the threat of digital eye strain (DES), making it an emerging public health problem.
/des.jpg)
Digital eye strains (DES) which also known as computer vision syndrome is defined by American Optometric Association, includes a range of visual and ocular symptoms occurred due to prolonged use of digital devices. Many studies suggest that the following factors are associated with DES, such as:
- screen glare (reflection from the digital display),
- poor lighting from the room or extensively exposure of lighting from the digital display,
- viewing digital screen from a wrong angle or distance,
- uncorrected vision problem (presbyopia, astigmatism, farsightedness),
- smaller font size
Viewing a digital screen for a few hours or more a day, or being too close to the digital device screen or having eye problems but did not correct with glasses or contact lenses, all these can worsen DES or causing recurrent of DES.
The symptoms of DES include eye dryness, eye fatigue, eye discomfort, eye redness, eye itching, blurred vision and headaches etc. The severity of visual symptoms of DES is based on the level of visual abilities and the amount of time spent on looking on the digital screen. Certain visual symptoms are temporary and will go away after the person stop using the digital devices, but some individual may still experience visual symptoms like blurred vision even after stop using digital devices. Symptoms may get worse if no steps taken to resolve the problem.
Treatments maybe vary for DES, but the symptoms can be relieved through optimal eye care and making changes in how the digital screen is viewed. Treatments include:
- After 2 hours of usage of digital devices, rest your eyes for at least 15 minutes
- Every 20 minutes, look into the distance at least 20 feet away from the computer or digital device. Do this for at least 20 seconds.
- Font size used in digital device should be enlarged.
- Digital devices should be positioned in a way to avoid glare, particularly from lighting of the room or lighting from windows.
- Digital devices should be viewed with the eyes looking downward. The digital screens are best to viewed at a 15 to 20 degrees below eye level and a distance of 20 to 28 inches from the screen (about an armlength)
- Remember to blink your eyes more frequently in order to minimize the risk of developing dry eyes when using a digital device as blinking can keep moisture on the eye’s surfaces.
Besides the changes which were stated above, management of eye dryness can help to treat or prevent the recurrent of DES due to dry eyes. For example, the use of lubricating eye drops to relieve the symptom of dry eyes. Lubricating eye drops can help to relieve symptoms of dry eyes, watery eyes or tired eyes, but it cannot completely cure DES, so only use eye drops when the symptoms are persistent. Some studies suggested dietary supplements such as omega-3 fatty acids and bilberry extract can help in relieving the symptoms of DES. These supplements have an important role in preserving the moisture levels in dry eyes conditions.
In conclusion, prevention is the most important step in management of DES. It involves the ensuring of an ergonomic work environment and practice as well as visual examination and eye care to treat visual disorders. Regular visual examinations can help to prevent or reduce the development of DES.
References
- Chaitra Jayadey, Puja Sarbajan, and Anand Vinekar (2020 Nov) Impact of the COVID-19 pandemic on digital eye strain in children. Indian Journal of Ophthalmology. 68(11): 2383-2384.
- Gammoh Y (February 26, 2021) Digital Eye Strain and Its Risk Factors Among a University Student Population in Jordan: A Cross-Sectional Study. Cureus 13(2): e13575. doi:10.7759/cureus.13575
- Pratyusha Ganne, Shaista Najeeb, Ganne Chaitanya, Aditya Sharma, and Nagesha C Krishnappa (2021) Digital Eye Strain Epidemic amid COVID-19 Pamdemic- A cross-sectional Survey. OPHTHALMIC EPIDEMIOLOGY 2021, VOL. 28, NO. 4, 285–292 https://doi.org/10.1080/09286586.2020.1862243
- Association AO. Computer vision syndrome. Accessed October 14 2020; Available from: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y
- Mark Rosenfield (Jan 2016) Computer vision syndrome (a.k.a. digital eye strain). Optometry in Practice 2016 Volume 17, Issue 1, 1–10
- Chantal Coles-Brennan, Anna Sulley and, Graeme Young. (2019) Management of digital eye strain. Clinical and Experimental Optometry 2019 ;102: 18-29

SLIPPED DISC

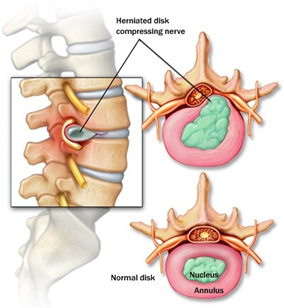
A slipped disc happens when one of the rubbery cushions (discs) that sit between the bones (vertebrae) that stack up spine pushes out from its position. The disc protects the bones by absorbing the shocks from daily activities like walking, lifting, and twisting.
Each disc has two parts: a soft, gelatinous inner portion and a tough outer ring. A slipped disc happens when the inner “jelly” substance pushes through the crack. This is also known as a herniated or prolapsed disc.
Causes
Several factors can contribute to a disc rupture, including:
- Aging – Disc becomes less flexible as people age and becomes more prone to tearing or rupturing
- Gender – Men between the ages of 20 and 50 are most likely to have a slipped disc
- Obesity – Excess body weight causes extra stress on the discs in the lower back
- Occupation – People with physically demanding jobs have a greater risk of back problems
- Sedentary lifestyle – Driving or working at a desk job for long time can increase the risk of a slipped disc
- Smoking – Less oxygen is supplied to the disc and it may lead to rapid degeneration of the discs

Symptoms
Slipped discs can happen anywhere along the spine, but slipped discs most often occur in the lower back or the neck. It’s rare for a slipped disc to be in the mid-back. However, not all slipped discs cause symptoms. Many people will never know that they have slipped a disc.
Slipped disc at the lower back
It’s common for a slipped disc at the lower back to cause “sciatic nerve” pain. This sharp pain usually radiates from the buttock to the leg and sometimes to the foot. Other symptoms of a slipped disc at the lower back include:
- Back pain
- Tingling or numbness in the legs and/or feet
- Muscle weakness
Slipped disc at the neck
Symptoms of a slipped disc at the neck include:
- Pain near or between shoulder blades
- Pain that travels to shoulder, arm and sometimes hand and fingers
- Neck pain, especially in the back and on the sides of the neck
- Pain that increases when bending or turning the neck
- Numbness or tingling in the arms
Treatment
In most cases, slipped discs do not require surgery. With time, the symptoms of a slipped disc will improve in approximately 9 out of 10 people. However, time taken to improve varies, ranging from a few days to a few weeks.
Nonsurgical treatment
Initial treatment for a herniated disc is usually nonsurgical. Nonsurgical treatment may include:
- Applying heat or cold. Initially, cold packs can be used to relieve pain and inflammation. After a few days, might switch to gentle heat to give relief and comfort.
- Rest. Take rest breaks throughout the day but avoid sitting for long periods. Try to avoid activities that worsen the pain.
- Resuming activity slowly. Make sure movements are slow and controlled, especially bending forward and lifting.
Medication
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as ibuprofen or naproxen can help relieve pain by treating inflammation in the nerves and soft tissues surrounding the disc.
- Neuropathic drugs. These drugs affect nerve impulses to decrease the pain. They include gabapentin (Neurontin), pregabalin (Lyrica), duloxetine (Cymbalta), or venlafaxine (Effexor XR).
- Muscle relaxants. These medications can calm spasms and ease pain. Sedation and dizziness are common side effects.
- Steroid injection. An injection of a cortisone-like medicine into the space around the nerve may provide short-term pain relief by reducing inflammation.
Physical therapy
Strengthening the core—the muscles in the back, abdomen, upper thighs, and buttocks—is an important part of therapy to treat symptoms of a slipped disc. If these muscles are weak, the spine bears more weight. This added pressure could cause instability or worsen an existing spine problem. A physical therapist can recommend a series of exercises for strengthening these core muscle groups, which can improve posture, relieve pressure on the nerves affected by a slipped disc, and alleviate pain.
Surgical treatment
A doctor may recommend surgery if conservative treatment options, such as physical therapy and medications, do not reduce or end the pain altogether. The benefits of surgery should be weighed carefully against its risks. Although a large percentage of patients with herniated discs report significant pain relief after surgery, there is no guarantee that surgery will help.
A patient may be considered a candidate for spinal surgery if:
- Pain limits normal activity or impairs quality of life
- Progressive neurological deficits develop, such as leg weakness and/or numbness
- Loss of normal bowel and bladder functions
- Difficulty standing or walking
- Medication and physical therapy are ineffective
- The patient is in reasonably good health
Complications
Left untreated, a slipped disc may lead to complications such as:
- Worsening symptoms, such as increased pain, numbness or weakness that can affect daily routine
- Loss of bladder control or bowel control, which may lead to incontinence or difficulty urinating
- Saddle anesthesia, where the slipped disc compresses the nerves and leads to loss of sensation in the inner thighs, back of the legs and around the rectum
- Permanent nerve damage, which may lead to permanent weakness or paralysis
Prevention
- Using proper lifting techniques
Position your feet shoulder-width apart
Bend your knees and keep your back straight
Use your legs to lift you up
Keep the object close to the center of your body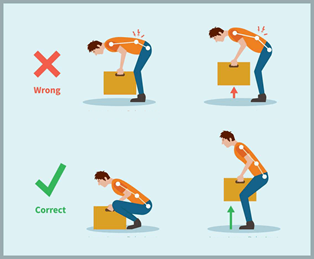
- Practicing good posture
When standing, keep your shoulders aligned over your hips
Avoid slouching, especially while sitting at your computer
Sit with your feet flat on the floor and your knees bent at 90-degree angles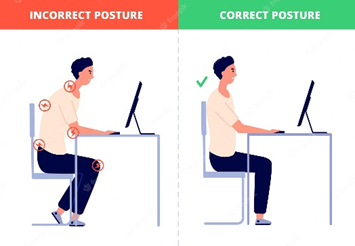
- Exercising regularly
- Focus on workouts that strengthen back and abdomen muscles to support your spine
Avoid exercises such as squats, sit-ups, and high impact aerobics activities
- Maintain a healthy weight
Being overweight or obese puts excessive pressure and strain on the back and knees. It also may contribute to poor posture
- Quit smoking
Smoking deprives healthy tissue of nutrients and oxygen, increasing the risk of developing spinal disc degeneration and osteoporosis. A smoker’s heavy coughing bouts can also increase pressure on the spine
References
Cleveland Clinic (2021). Herniated Disk (Slipped, Ruptured or Bulging Disk). Retrieved 10 June 2023, from https://my.clevelandclinic.org/health/diseases/12768-herniated-disk .
Mayo Clinic (2022). Herniated disk. Retrieved 10 June 2023, from https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095 .
Nall, R. (2017). Slipped (Herniated) Disc. Retrieved 10 June 2023, from https://www.healthline.com/health/herniated-disk .
Park, D. K. (2022). Herniated Disk in the Lower Back. Retrieved 10 June 2023, from https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disk-in-the-lower-back/ .
Portal Rasmi MyHEALTH (2019). Slipped Disc of Spine. Retrieved 10 June 2023, from http://www.myhealth.gov.my/en/slipped-disc-spine/ .