Introduction
Infertility is now a concerning health issue among Malaysian couples with a raising number on statistical charts . We often oversee that it may not just involve women, but men as well.
According to Deputy Minister of Women, Family and Community Development Malaysia, infertility problem among men in Malaysia is at an alarming level. Based on sperm analysis data from the National Population and Family Development Board, 60% of the test showed abnormal results.
What is infertility?
Infertility is defined by the failure to achieve pregnancy (conceive) even after a year of unprotected sex. It can be caused by female or male issues. If you are infertile, don’t panic as there are many options available today in Malaysia. No matter what the issue is, and whether it is male or female infertility, there is a way to have your baby. You are advised to meet a fertility doctor if you have been trying to get pregnant for the past one year and still couldn’t conceive.
What causes infertility?
Infertility may be caused by many reasons. It is important for you to understand them while planning for pregnancy.
Common reasons for infertility in women:
- Ovulation disorders can lead to irregular menstrual cycle. It could be induced by hormonal disorders such as polycystic ovary syndrome (PCOS), hyperprolactinemia, hyperthyroidism or hypothyroidism.
- Uterine or cervical abnormalities may affect embryo implantation and development in the uterus.
- Damaged or blocked fallopian tube may prevent fertilization or even when it happens, the fertilized egg might fail to reach the uterus.
- Endometriosis occurs when endometrial tissue grows out of the uterus and affect the function of ovaries, uterus and fallopian tubes.
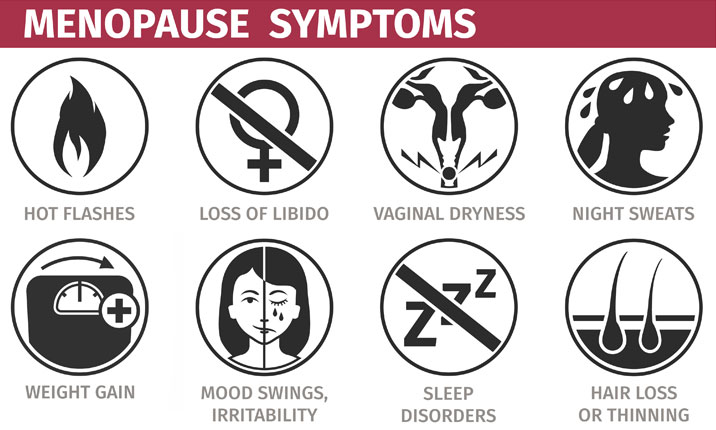
- Primary ovarian insufficiency (early menopause) where the ovaries stop working and menstruation ends before the age of 40.
Common reasons for infertility in men:
- Abnormal sperm production or function
- Problems with delivery of sperm, such as premature ejaculation.
- Over–exposure to certain environmental factors, such as pesticides, chemicals, radiation and cigarette smoke.
- Poor lifestyle such as habitual intake of alcohol, marijuana, steroids may affect sperm production and quality.
What increases the risk of infertility in women and men?
Risk factors for infertility among both women and men are similar. They include:
- Age factor, where fertility gradually decreases in both female and male as they age, especially in women as the approach the menopausal age.
- Smoking.
- Excessive alcohol consumption.
- People who are overweight, obese or underweight.
- Exposure to environmental toxins including pesticides, lead or mercury may cause infertility or birth defects.
- Excessive physical or emotional stress may result in amenorrhea in women.
- Frequent exposure of the testes to high temperatures, frequent sauna or hot tub use can cause infertility in men.
How to treat female infertility?
Methods that can be used are:
- Stimulating ovulation with fertility drugs. For example, Clomiphene Citrate. You can consult a doctor before taking this medicine.
- Intrauterine insemination (IUI). During IUI, healthy sperms are placed directly into the uterus when ovary releases one or more eggs to be fertilized.

Intrauterine insemination (IUI)
- Assisted Reproductive Technology (ART). In-Vitro Fertilization (IVF) is the most common ART technique. IVF involves stimulating and retrieving multiple matured eggs, fertilizing them with sperm in a dish in a lab, and implanting the embryos in uterus several days after fertilization.

In-Vitro Fertilization
- Planning pregnancy using Timed Intercourse method. It is a cost-effective method which is suitable for couples where the woman partner does not have any issues with her uterus and fallopian tube, and the male partner does not have any issues with his sperm. This method refers to having intercourse during times when the chances to get pregnant are the highest. It is encouraged to have regular intercourse several times around the ovulation period (on the 14th day of menstrual cycle). You may have your intercourse at least five days before and until a day after ovulation to improve your chances of getting pregnant.
How to treat male infertility?
Methods that can be used are:
- Surgery. In some conditions, surgery may be able to reverse a sperm blockage and restore fertility.
- Sperm retrieval. This technique can be used when ejaculation is a problem or when no sperms are present in an ejaculated fluid. They may also be used in cases where assisted reproductive techniques are planned and sperm counts are low or abnormal.
- Changing lifestyle. Avoid smoking, excessive alcohol consumption, excessive exposure to radiation or heat.
Tips to prevent infertility
Women
- Exercise moderately.
- Good weight management
- Limit caffeine intake.
- Quit smoking.
- Avoid alcohol consumption.
Men
- Avoid drug and tobacco use and drinking too much alcohol.
- Avoid high temperatures whilst in hot tub and hot bath.
- Avoid exposure to industrial or environmental toxins
- Exercise moderately.
How to cope with the journey to get pregnant?
Coping with the journey to get pregnant can be long and stressful. The process of assisted reproduction itself can lead to psychological distress. It can induce stress, anxiety and depression. These are few tips for you to try and follow:
- Be prepared. Infertility tests and treatments can be difficult and stressful. You can always seek professional help to get insights about the procedures to be mentally and physically prepared.
- Set limits. Discuss with your partner on the limits to try for it and know about your financial level. Fertility treatments could be expensive and repeated attempts may be required to achieve successful pregnancy.
- Seek emotional support when required.
- Exercise moderately and eat healthy.
Reference
https://www.mayoclinic.org/diseases-conditions/infertility/diagnosis-treatment/drc-20354322
https://bestpractice.bmj.com/topics/en-us/498https://www.thestar.com.my/news/nation/2023/04/05/fertility-problems-among-men-in-malaysia-alarming-says-deputy-minister